Better cancer care for members. Lower costs for partners.
Thyme Care delivers comprehensive cancer care navigation and wraparound clinical support, coordinating care for members with cancer to enhance outcomes and experiences while reducing the total cost of care.

Personalized, wraparound support members deserve.
With 24/7 access to a virtual, expert Care Team, Thyme Care ensures members have someone in their corner for everything they need to navigate their cancer journey.
24/7 Comprehensive Support
Dedicated, oncology-trained Care Team provides personalized support from pre-diagnosis through survivorship. Members can access their Care Team at any time, with on-demand resources available via our digital platform, Thyme Care Connect.
Proven Cost Reduction
Ongoing symptom monitoring and an intelligent care delivery platform enable our Care Team to anticipate member needs before they arise, deploying proactive support to reduce acute care costs. Partnerships with select oncology groups unlock additional value and reduce drug spend.
Close Provider Collaboration
Thyme Care works directly with a member’s oncologist across all settings, serving as a practice extension for coordinated, enhanced support and ensuring continuity of care throughout the cancer journey.
In collaboration with:


Driving meaningful results for our partners and their members.
15-20%
Reduction in acute care spend
9/10
Thyme Care member satisfaction rate
72%
Mobile symptom ID member response rate
8 million
Members have access to Thyme Care services
*The information presented on this website is based on a difference-in-differences study using medical claims exclusively from a regional Medicare Advantage plan. As such, the study excludes the impact of additional interventions that Thyme Care deploys for other segments, and new interventions that Thyme Care has launched since. Contact us to evaluate the value Thyme Care can drive for your population.
Thyme Care is transforming the cancer care experience.
Our comprehensive oncology care solution lowers cancer care costs while improving member experience and satisfaction.
The Thyme Care Model
Thyme Care partners with health plans and other risk-bearing entities to assume accountability for enhanced care quality, improved health outcomes, and reduced cost of care for their cancer populations.
Assess
Our analytics platform enables savings forecasting and value delivery by aligning incentives and assuming population risk for all actively treated cancer patients, regardless of their treating oncologist.
Deploy
Together, we’ll tailor incentives and implement a care model that integrates into your existing processes, teams, and network to meet the specific needs of your plan, providers, and members.

Deliver
We will begin supporting the delivery of high-touch, whole-person cancer care to your members within months, driving improved outcomes and experience while reducing cost of care.
Intelligent care that meets members where they are.
Thyme Care assists members throughout their cancer journey, delivering personalized, data-driven care guidance to improve member outcomes and experience.
-
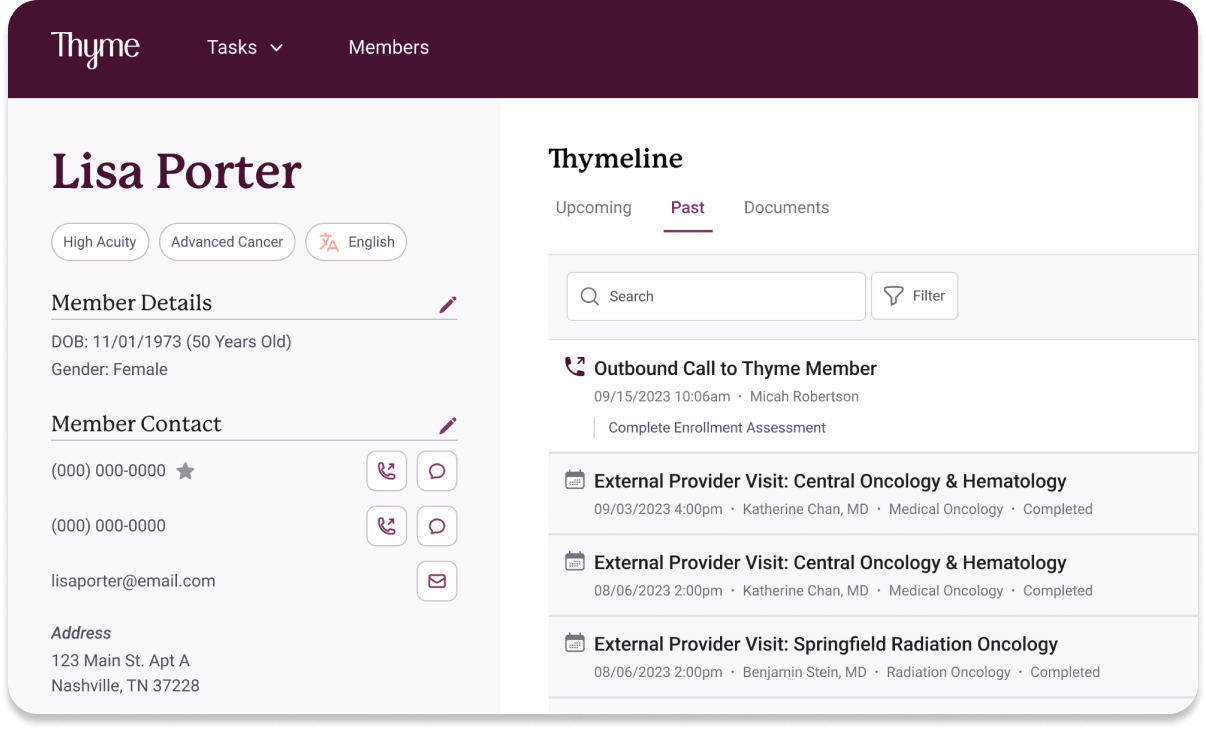
Meet Lisa
Lisa is a 60 year-old woman recently diagnosed with breast cancer. Her oncologist tells her she is eligible for support from Thyme Care and refers her into the program that same day.

-
Pre-populated patient profile
Using claims, HIE and EHR data integrations, Lisa’s information is automatically pre-populated into Thyme Box, Thyme Care’s care delivery platform, so that her Care Team has a full picture of her needs and circumstances.
-
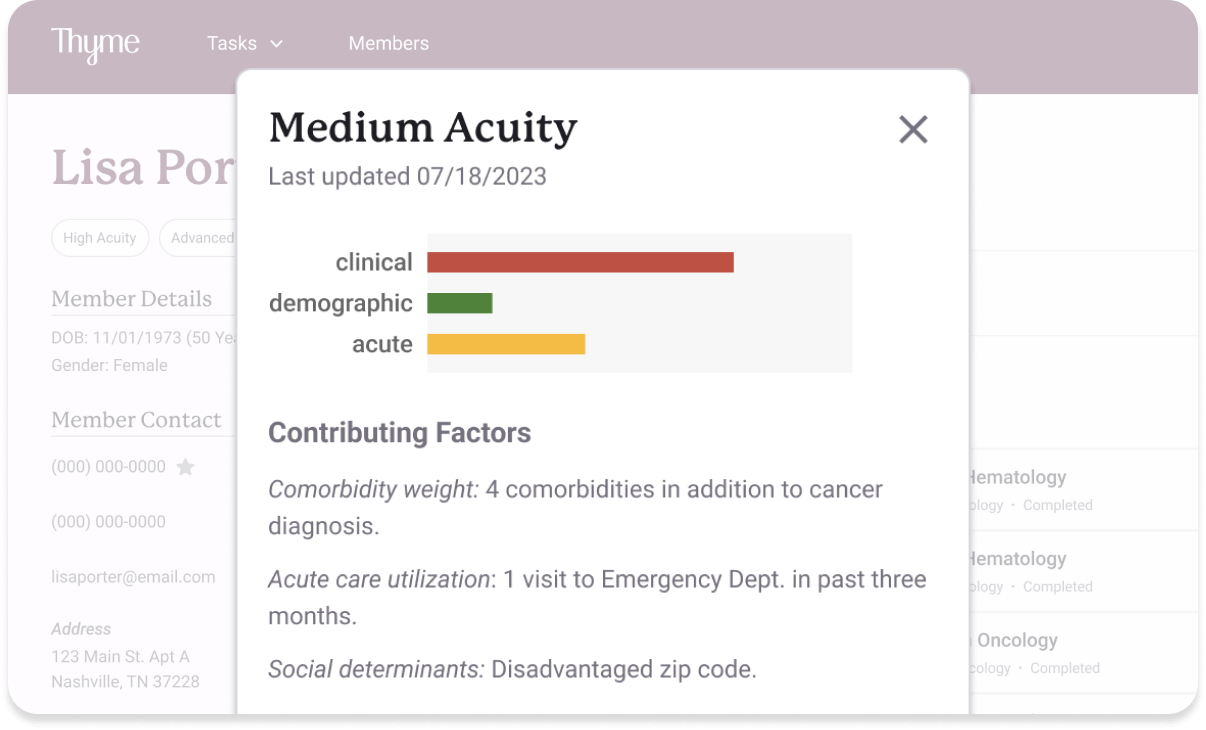
Advanced acuity scoring
Lisa’s information is also fed into Thyme Care’s analytics platform which auto-generates an acuity score to inform her care plan.
-
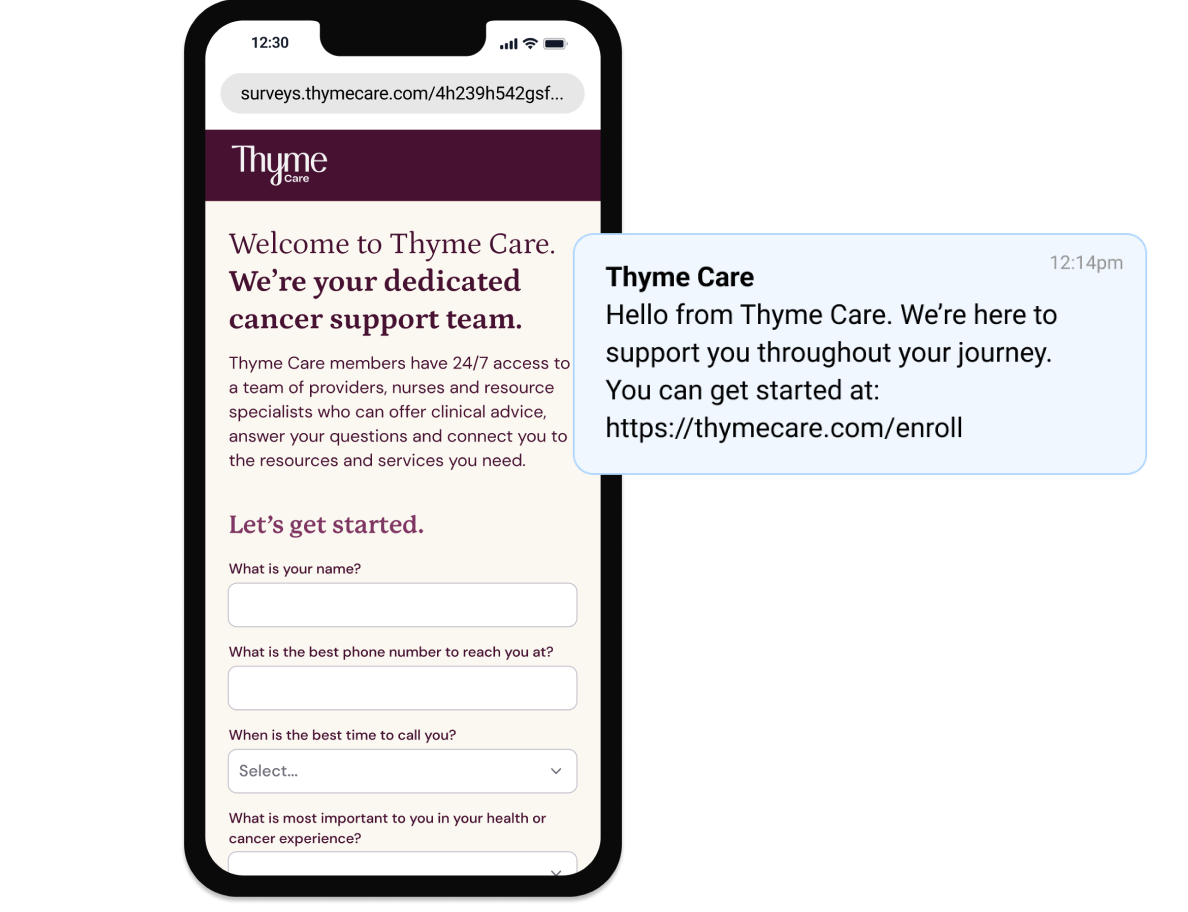
Distress Thermometer
Lisa receives a text from Thyme Care with a link to complete a brief monthly check-in on her symptoms and emotional wellbeing.
After reporting a high symptom score, she gets a follow-up from the Care Team. Lisa can also use Thyme Care Connect, a web-based app, for additional self-service support.
-
Personalized social needs support
In the follow-up call with her Care Partner, Lisa shares that she wants to delay treatment due to cost concerns.
Her Care Partner identifies and helps her apply for a breast cancer specific grant to ease the financial burden and also coordinates with her treating oncologist to schedule treatment.
-
Intelligent symptom monitoring
On day 3 of treatment, Lisa experiences side effects and goes to Thyme Care Connect to educate herself on what to expect and ways to proactively manage any adverse reactions. She also fills out a Symptom Assessment.

-
Wraparound clinical support
Lisa’s elevated nausea score triggers an alert to a Thyme Care Nurse, who calls and identifies dehydration.
Thyme Care coordinates with her oncologist to provide same-day IV hydration and antiemetics, avoiding an ED visit.
The EHR integration ensures the details are automatically shared with her oncology practice to improve continuity of care.

24/7 member support, delivered in coordination with oncologists.
All members receive our 24/7 wraparound cancer care support, regardless of oncology provider or setting. Thyme Care further enhances the member experience by working directly with the member’s treating oncologist or through our deeply integrated oncology partnerships.
Collaborating with a member’s oncologist
We coordinate with your member’s treating oncologist in hospital and community practice settings to ensure continuity of care and share back relevant information for seamless coordination.
Extending care through Thyme Care Oncology Partners (TCOP)
Thyme Care partners with oncology groups across the nation (TCOP). In addition to coordinating care, our TCOP helps amplify the impact of our model, unlocking additional interventions and value for your organization.
Learn more about the benefits here.

.png)
.png)